Poison in the Fields: The Glyphosate Gamble
Case from the ICU Desk – CriticalICU
Case Summary
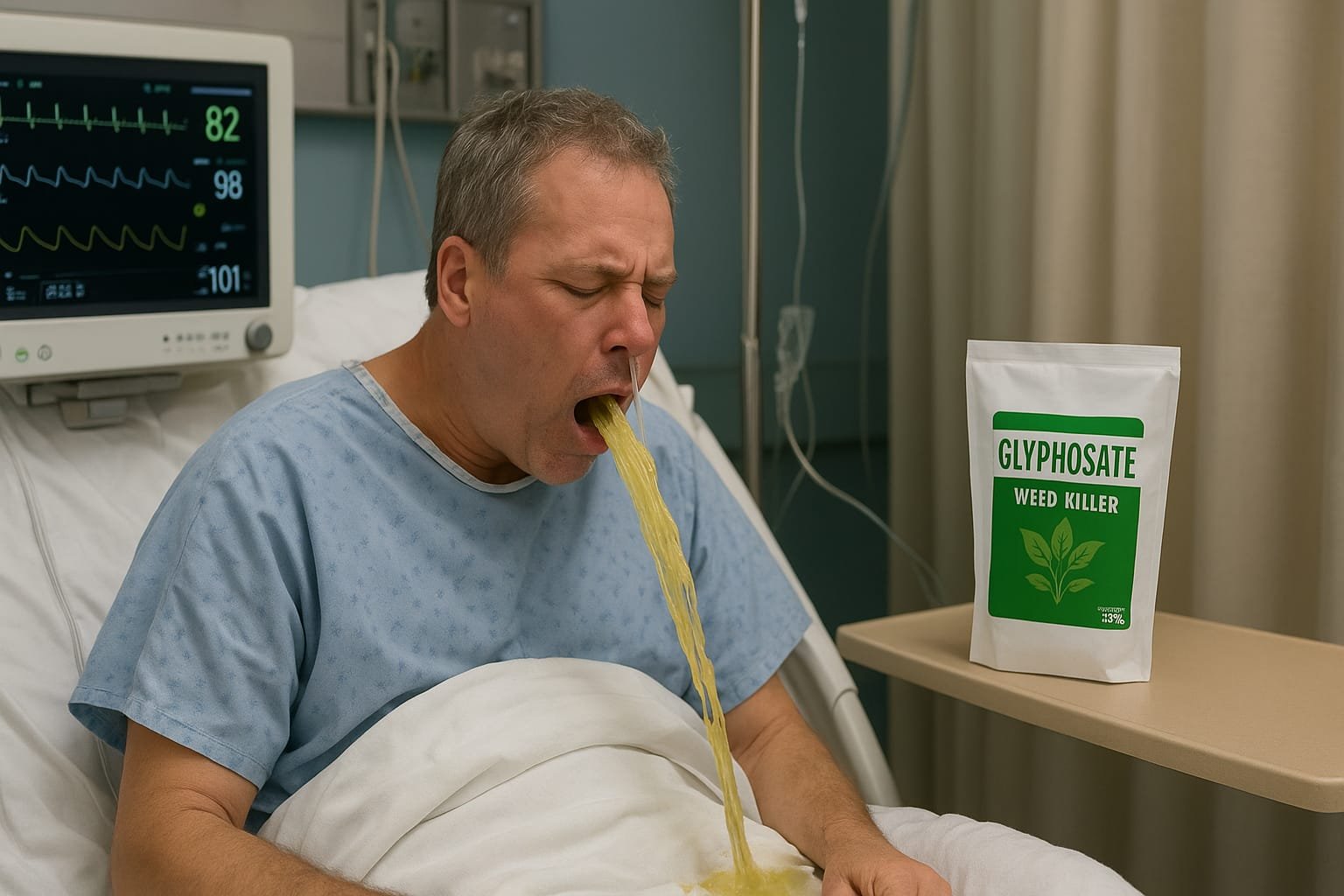
A 38-year-old male, known case of Diabetes Mellitus and Ischemic Heart Disease, presented to the emergency department after ingesting ~80 g of ammonium salt of glyphosate (71%), a common herbicide.
He arrived fully conscious, oriented, afebrile, but with persistent vomiting.
Background
Glyphosate, though widely marketed as “low toxicity”, can be life-threatening when ingested in large amounts—especially formulations with surfactants like polyethoxylated tallow amine (POEA).
Unlike organophosphates, glyphosate does NOT inhibit cholinesterase—but can cause multi-organ failure, hypotension, ARDS, and metabolic acidosis.
On Arrival — Vitals & Investigations
Neurological: Pupils 1 mm, reactive to light. No fasciculations.
GIT: Repeated vomiting, no diarrhea.
Renal: Foley inserted; baseline creatinine 1.13 mg/dL.
Liver: Mildly elevated SGOT/SGPT (49/56 IU/L).
Hematology: Hb 15.8 g/dL, WBC 6590, Platelets 1.11 lakh/µL.
Metabolic: RBS 237 mg/dL (stress hyperglycemia + DM).
Phosphate: 100 µmol/L – within normal range.
ABG:
pH: 7.35 (borderline acid-base status)
HCO₃⁻: 20.9 mmol/L (mild metabolic acidosis)
Lactate: 2.0 mmol/L (slight tissue hypoperfusion possible)
Cholinesterase: 510 U/L – normal, ruling out OP poisoning.
ECG: Normal sinus rhythm, no ischemic changes.
Chest X-ray: Clear lung fields, no infiltrates or edema.
Reasoning & Justification of Treatment
- Gastric Decontamination
- Ryle’s tube lavage was performed until clear return.
- Justification: Early (<1 hr) gastric lavage may reduce systemic absorption, but is controversial; here, done promptly after arrival.
- Activated charcoal was avoided because glyphosate binding is poor and patient was vomiting.
- Supportive Therapy
- NBM to prevent aspiration risk & allow gut rest.
- IV fluids @100 ml/hr — to maintain hydration & protect kidneys (glyphosate may cause AKI due to hypotension and direct tubular injury).
- Symptom Control
- Inj. Emset (Ondansetron) 4 mg IV TDS – antiemetic to control vomiting.
- Syp Sparacid – antacid + mucosal protective agent for gastritis risk.
- Inj. Pantoprazole – gastric acid suppression & mucosal protection.
- Antibiotic (Inj. Monocef 2 g IV BD)
- Prophylactic coverage due to Ryle’s tube, Foley catheter, and aspiration risk. Not routine in all poison cases, but justified here given comorbidities and invasive lines.
- Monitoring
- ABG & Lactate to track acid-base shifts.
- Electrolytes & Renal/Liver function every 12–24 hr.
- Cardiac monitoring — patient with IHD; arrhythmias can be precipitated by electrolyte imbalance.
Differential Considerations
- Organophosphate Poisoning – ruled out by normal cholinesterase.
- Other herbicides (Paraquat, 2,4-D) – more severe lung/kidney injury; here presentation was milder.
Pertinent Positives & Negatives
| Finding | Positive in this case |
| Vomiting | YES |
| Hypotension | NO |
| Acidosis | YES MILD |
| Renal Failure | NO |
| CNS Depression | NO |
| Pupil Size | 1 MM REACTING |
| Cholinergic signs | NORMAL |
Toxicology Pearl
Glyphosate toxicity severity correlates with amount ingested, surfactant presence, and time to treatment. Mortality rises when ingestion >85 mL (about 70–80 g solid equivalent) and in elderly or comorbid patients.
Mini Story — “The Farmer’s Gamble”
It was just another hot afternoon in the fields when Mr. R, frustrated with debts, reached for a shiny yellow herbicide packet. Minutes later, waves of nausea and regret hit harder than the summer sun.
In the ICU, his first words were not about pain, but about how bitter it tasted.
The team moved swiftly—gastric tubes, IV lines, antidote hunt (none for glyphosate), and monitors blinking in quiet defiance.
By the end of the shift, his vomiting slowed, vitals stayed stable, and the fight—at least for now—was in his favor.
Quick Q&A
- Qus: Why is atropine not indicated here?
Ans: Atropine treats muscarinic excess in organophosphate poisoning. Glyphosate does not cause cholinergic crisis. - Qus: What’s the mainstay of treatment?
Ans: Aggressive supportive care — airway, breathing, circulation, fluids, and symptom control. No specific antidote exists.
Key Takeaways
No antidote for glyphosate — supportive care saves lives.
Always differentiate from OP poisoning with cholinesterase levels.
Watch for AKI, ARDS, refractory hypotension in first 48 hours.
Early gastric lavage may be useful if done within 1 hr and patient is conscious.
Sources
Bradberry SM et al. Glyphosate poisoning. Toxicol Rev. 2004.
Eddleston M et al. Herbicide Poisoning. N Engl J Med. 2008.
WHO Recommended Classification of Pesticides by Hazard, 2020.
CDC – Toxic Substances Portal, Glyphosate